
Recurrent miscarriages affects 1-2 percent of reproductive age women. However in India the prevalence is 7.4%. Researchers have been intrigued by the complexity of the factors causing it and treatment that may help to prevent or manage it. It is important for clinicians to be updated with the evolving investigations and evidence based treatment options to mange couples with recurrent miscarriages.
ESHRE/ RCOG/ASRM/MOHFW: Depending upon the gestation of viability and epidemiological data each society has different definition of Miscarriage and RM (Recurrent Miscarriages)
GDG of ESHRE Defines: A pregnancy loss is defined as the spontaneous demise of a pregnancy before the fetus reaches viability. The term therefore includes all pregnancy losses from the time of conception until 24 weeks of gestation.
The term Recurrent Pregnancy Loss for two or more pregnancy loss and to reserve ‘recurrent miscarriages’ to describe cases where all pregnancy losses have been confirmed as intra-uterine miscarriages.
RCOG: Uses 24 weeks as the cut off for viability and defines recurrent miscarriages as the loss of three or more consecutive pregnancies (< 24 weeks).
MOHFW: Miscarriage is defined as a spontaneous loss of pregnancy before 20 weeks of gestation.
Recurrent Miscarriages: Women with three or more first trimester and one or more second trimester miscarriage. Early evaluation is considered if fetal cardiac activity was present, women >35 years with two or more abortions and the couple has had difficulty in conceiving. Women with two or more losses with one or more live issues should be excluded.
ASRM: Recurrent pregnancy loss is two or more failed pregnancy where pregnancy means a clinical pregnancy documented by ultrasound or histopathology.
Working definition warranting investigation & work up and management accordingly.
Miscarriage: Any pregnancy loss from conception till the fetus reaches viability (<24 weeks) Couples with more than two miscarriage should be evaluated consecutively or non consecutively. This would include clinical and biochemical pregnancies but excludes ectopic, molar pregnancies and implantation failure in ART.
In absence of adequate data on the effect of a non consecutive pregnancy loss on the subsequent pregnancy, they should not be clearly excluded from evaluation. Although no distinction in the definition criteria for first or second trimester loss in made but any obvious factor leading to pregnancy loss should not be ignored.
Terminology like Primary RPL (multiple losses in a woman with no previous viable infants) secondary RPL (multiple losses in a woman who has already had a pregnancy beyond 20 gestational weeks) and Tertiary RPL (multiple pregnancy losses between normal pregnancies) are clinically irrelevant for investigating a case of RPL.
Ideally there should be dedicated RM Clinic which in-depth investigates the couples with recurrent miscarriages. Clinicians and clinics should take the psychosocial needs of couples faced with RM into account when offering and organizing care for these couples. Investigations need not necessarily lead to treatment options and this should be explained to the couple from the beginning. The prognosis and recurrence prediction charts should be used to counsel the couples and overall the chances of successful live birth after RM are satisfactory.
What are the Risk Factors for having RM: Recurrent miscarriages are associated with following risk factors. Some of them are modifiable and adoption of health changing behavior can lead to definitive reduced risk of another miscarriage. While for other non modifiable factors various treatment modalities have been tried but only a few can be recommended to be used based on the scientific literature published.
BMI: Maternal obesity has a strong association with repeated miscarriages but the direct effect of weight loss in achieving live birth is not studied. But weight loss definitely decreases time to conceive and risk of miscarriages and other medical obstetric complications like pregnancy induced hypertension, diabetes and metabolic syndrome in general. Also on the other hand a BMI of less than 18.5 is found to be associated with sporadic first trimester losses. Achieving optimal BMI should be a treatment goal in management.
Exercise in pre pregnancy and during pregnancy is found to have no negative effect on the pregnancy outcome rather it benefits by improving tissue oxygenation and helping achieve normal BMI.
Smoking: Smoking has not been conclusively found to be a risk factor for RM but based on its definitive association with poor obstetric outcomes, cessation of smoking should be advised in couples with RPL even in absence of data supporting smoking cessation and chance of live birth.
Caffeine: A study on small population found a linear correlation between the amount of caffeine intake in pre-pregnancy and early pregnancy period and pregnancy loss, maximum being with >300mg/day of caffeine consumption compared to mild consumption > 150 mg/day. However the chances of live birth on caffeine intake reduction is not studied.
Alcohol: Alcohol consumption is associated with pregnancy loss and fetal alcohol syndrome. Seeing the negative effects of alcohol even in absence of direct causal relation it is advised to limit or curtail alcohol consumption in the pre-conceptional period.
Stress: Stress is associated with RPL but direct causative relation has not been established due to non-uniformity in type of scales used and poor study designs.
Endometritis: Very small studies have found the presence of endometritis in women with RPL and improving with antibiotic treatment, however these studies are inadequately designed to form basis for screening for endometritis.
Age: Advanced female age is associated with sub fertility, genetic anomalies, obstetric complications, still births etc. The risk of another miscarriage in woman with RPL has been found to double after the age of 35 years. Woman should be told that the risk of RPL is lowest between 20-35 years and rises rapidly after 40 years.
Occupational and environmental exposure: Based on only a few small studies, exposure to occupational and environmental factors (heavy metals, pesticide, lack of micronutrients) seems to be associated with an increased risk of pregnancy loss in women with RPL.
Genetic: Majority of early pregnancy losses (50%-60%) are due to chromosomal abnormalities resulting as a de novo process or are parental in origin. Most common parental abnormalities leading to miscarriages are translocations (2-4%) which can be Reciprocal (60%) equal exchange of genetic material between two chromosomes or Robertsonian (40%) where long arm of two acrocentric chromosomes join together. Carrier parents are asymptomatic. These can be picked up by karyotyping of parents. The karyotype of products of conception can be normal or have a balanced or an unbalanced translocation. Pregnancies with unbalanced translocations usually end in miscarriage, still births and rarely anomalous babies.
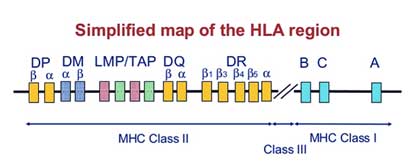
Immunological: The association between HLA (Human Leucocyte antigen) polymorphism and RM is inconsistent. Of the various types a weak association is found between HLA-G alleles with RM. Investigation of HLA in women with RM is not recommended except class II HLA in women with secondary RPL after the birth of a boy.
There should be individual evaluation of the investigations appropriate to each woman or couple, based on age, fertility/sub-fertility, pregnancy history, family history, previous investigations and/or treatments. In addition, care should be tailored to the psychological needs of the couples.
Products of Conception: Aneuploidy is the most common cause of early pregnancy losses and the risk increases with age of the woman. Aneuploidies occur in comparable frequencies in both women with sporadic and recurrent pregnancy loss. Although not mandatorily recommended but genetic analysis of the products of conception help in explanatory purpose and may help to determine whether further investigations or treatments are required. For Genetic analysis of POCs array CGH is recommended.
Parental Karyotype: The test should be advised only after individual risk assessment. Parental karyotyping is advised based on genetic history (history of previous child with congenital abnormalities, offspring with unbalanced chromosome abnormalities in the family, or detection of a translocation in the pregnancy tissue). In couples with female age above 39, less than three pregnancy losses and a negative family history, the chance of being a carrier of a translocation is very low.9 The information from parental karyotype however helps couples in deciding continuing to try to conceive, stop trying, or choose invasive tests like prenatal diagnosis or preimplantation genetic testing (PGT) (for instance PGT-SR in case of a balanced translocation)
Acquired : Antiphospholipid antibody syndrome is associated with RM by action of anti PL in complement activation and vascular thrombosis. The Miyakis criteria (2006), an update of the Sapporo classification of 1999, is used to diagnose antiphospholipid antibody syndrome. This requires presence of one clinical criteria and elevated levels of aPL antibodies. (box) Screening for antiphospholipid antibodies, Lupus anticoagulant, Anti cardiolipin antibody and aβ2GlycoProtein I should be considered after two pregnancy losses at least 6 weeks after a miscarriage.
Hereditary: There is no, or a weak association at best, between RPL and hereditary thrombophilia. It is hence not recommended to screen for hereditary thrombophilia in women experiencing RPL however in presence of additional risk factors for hereditary thrombophilia like family members with hereditary thrombophilia, or previous VTE, screening can be considered.
Presence of uterine malformations is more common in woman with RM. The association is strong for congenital than acquired ones and treating them has improve live birth rates in some studies. All women with RM should be screened for malformations. The preferred technique to evaluate the uterus is transvaginal3D ultrasound (3D US), which has a high sensitivity and specificity compared to a 2D US. Sonohysterography (SHG) is more accurate than hysterosalpingography (HSG) in diagnosing uterine malformations more so when tubal patency has to be investigated. MRI is not the first line investigation.
Congenital Abnormalities: Potentially relevant congenital Müllerian tract malformations include septate uterus, bicorporeal uterus with normal cervix (AFSbicornuate uterus), bicorporeal uterus with double cervix (AFSdidelphic uterus) and hemi-uterus (AFSunicornuate uterus).
Acquired Abnormalities: Acquired uterine malformations (submucousal myomas, endometrial polyps and uterine adhesions) have been found prevalent in women that suffered pregnancy loss, but the clinical relevance is unclear. 3 D USG is a better screening tool. When suspected, a hysteroscopy has to be performed. It is the gold standard.
Cervical Incompetence: Women with a history of second-trimester pregnancy losses and suspected cervical weakness should be offered serial cervical sonographic surveillance.
Thyroid &antoTPO, Diabetes Mellitus, Androgens &LH: Thyroid screening (thyroid-stimulating hormone [TSH] and thyroid peroxidase [TPO]-antibodies) is recommended in women with RPL. Abnormal thyroid-stimulating hormone (TSH) and thyroid peroxidase [TPO]-antibody levels should be followed up by thyroxine (T4) testing in women with RPL. Assessment of polycystic ovary syndrome (PCOS), fasting insulin and fasting glucose, baseline androgen levels and LH is not recommended in women with RPL to improve next pregnancy prognosis. However prolactin testing should be undertaken in symptomatic women (Oligo/amenorrhoea). Routine testing for luteal phase insufficiency in neither feasible nor necessary in women wit RM.
HLA determination in women with RPL is not recommended in clinical practice.
List of tests & Recommendations (Table)
| Test | Recommendation |
|---|---|
| anti-HY antibodies | Not recommended |
| Cytokine testing | Not recommended |
| Cytokine polymorphisms | Not recommended |
| Antinuclear antibodies (ANA) testing | Could be considered for explanatory purpose |
| natural killer (NK) cell testing | Insufficient evidence to recommend |
| anti-HLA antibodies | Not recommended |
The role of male factor in RM is being investigated owing to the fact that female causes explain only about 50-60% cases of RM.
Assessment of spam DNA fragmentation can be considered for explanatory purposes not therapeutic purpose based on indirect evidence.
Endometrial aspiration to screen for endometritis is not recommended due to lack of evidence and the diversity of nature of infectious agent being studied and treated in various studies.
Introduction: The treatment in RM could be specific in 50-60% cases where aetiology is identified by the extensive work up the couple undergoes or it is empirical as used in the remaining 40-50% cases of unexplained RM. In either scenario the psychological needs and expectation of the couple from treatment should be well dealt.
Prognosis: Couples are keen to not only know the cause but also the chances of recurrence of such an event in case specific manner. Few prognostic tools (Lund and Brigham) were evaluated, that is female age, number of preceding losses can guide about the prognosis.
Treatment options specially the empirical ones or the ones with insufficient evidence should be offered based on reasonable pathophysiological hypothesis and after adequate information to the couple.
Role of PGT-M and PGT-SR: Preimplantation genetic testing for monogenic/single gene defects (PGT-M) or chromosomal structural rearrangements (PGT-SR), previously PGD, is an established method to preconceptionally select the genetic defect free embryo for transfer in couples with a high risk of transmitting genetic disorders.Structural chromosomal defects are common in RM population and PGT is useful in couples who are carrier of translation to prevent miscarriage although this is backed by limited evidence and lack of RCT’s
All couples with abnormal genetic results from pregnancy tissue testing or parental karyotypes should be offered genetic counseling to discuss likely prognosis and further diagnostic options. In addition, couples should be informed that PGT-SR could reduce the miscarriage rate, but will not improve live birth rate or time to pregnancy.
Role of PGT-A in unexplained RPL: Preimplantation genetic testing for aneuploidy (PGT-A) (previously preimplantation genetic screening [PGS] or preimplantation diagnosis of aneuploidy [PGD-A]), where an IVF cycle creates embryos which are biopsied and screened for chromosomal anomalies prior to implantation, has been proposed as a potential treatment for RM. However systematic reviews on PGS (PGT-A) for unexplained RM concluded that there is no improvement in live birth rate and hence not cost effective.15
Role of Anticoagulants: Aspirin & LMWH
APS: Women who fall under the diagnosis of APS based on the criteria are advised to take low dose aspirin (75-100mg/day) before conception and prophylactic dose of LMWH or unfractionated heparin from the day of pregnancy test positive. For women with hereditary thrombophilia and a history of RPL, antithrombotic prophylaxis is not recommended unless in the context of research, or for venous thromboembolism (VTE) prevention.
No role of steroids or IvIG for this indication
Diagnosis of immunological cause is a dilemma and in absence of clear evidence no specific treatment can be recommended.
| Procedure with RM | Recommendation |
|---|---|
| Hysteroscopic septum resection | Needs evaluation for RM (ESHRE). But GPP should be done |
| Metroplasty for bicorporeal uterus with normal cervix | Not recommended |
| Uterine reconstruction for hemiuterus | Not recommended |
| Metroplasty in women with bicorporeal uterus and double cervix | Insufficient evidence |
| Hysteroscopic removal of submucosal fibroids or endometrial polyps in women with RPL | Insufficient evidence but GPP should be done |
| Surgical removal of intramural fibroids | Not recommended |
| Im fibroid distorting the cavity | Insufficient evidence GPP: decision should be individualized |
| Surgical removal of intrauterine adhesions | Insufficient evidence |
| Cervical cerclage : singleton pregnancy and a history of recurrent second-trimester pregnancy loss attributable to cervical weakness | Recommended |
| Lymphocyte immunization therapy | Should not be used, may have serious adverse effects |
| Intravenous immunoglobulin (IvIg) | Not recommended |
| Glucocorticoids | Not recommended |
| Heparin or low dose aspirin | Not recommended |
| Folic Acid | Not recommended for RM prevention, given routinely to prevent NTD |
| Vaginal progesterone | Insufficient evidence |
| granulocyte- colony stimulating factor (G-CSF) | Insufficient evidence |
| Intralipid therapy | Insufficient evidence |
| Endometrial Scratching | Not recommended |