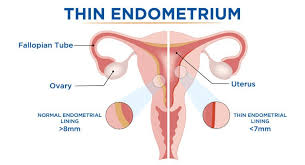
Thin Endometrium – causes and treatment
Thin endometrium is a medical condition affecting women, characterized by a thinning of the uterine lining (endometrial lining), which can impact fertility and pregnancy outcomes. Understanding its causes and available treatments can help manage this condition effectively.
Types and Causes of Thin Endometrium
1. Structural Factors
Structural abnormalities can reduce blood flow to the uterus, leading to a thinner endometrial lining. Common structural causes include:
Uterine growths that interfere with endometrial lining development.
Scar tissue formation in the uterus that causes endometrial thinning.
A bacterial infection that damages the uterus and hinders endometrial growth.
Treatment Options for Structural Factors:
A surgical procedure to remove polyps and scar tissue using a small camera.
Prescribed for tuberculosis-related uterine damage.
Medications to boost endometrial growth during the luteal phase of the menstrual cycle.
2. Hormonal Factors
Hormonal imbalances can disrupt estrogen and progesterone levels, essential for a healthy endometrial lining.
A shorter luteal phase negatively affects endometrial growth.
Caused by premature ovarian failure, menopause, or other hormonal issues.
Treatment Options for Hormonal Factors:
Medications to restore estrogen and progesterone levels.
Additional hormone support to encourage endometrial thickening.
3. Immune Factors
Immune system issues can prevent the uterus from supporting pregnancy, contributing to a thin endometrium.
A critical process involving the placenta-forming cells and the endometrial lining.
A protein influencing immune response and endometrial development.
Treatment Options for Immune Factors:
Stimulates new cell growth by gently scratching the uterine lining.
Medications to boost GCSF levels and improve endometrial growth.
Injections created from the patient’s blood to stimulate endometrial growth.
Additional Treatment Options
Medications can enhance uterine blood flow, assessed by color Doppler ultrasound.
Postponing embryo transfer until the lining reaches optimal thickness.
Performing FET when the endometrial lining is adequately thickened.
By identifying the underlying causes and selecting appropriate treatments, managing thin endometrium becomes more effective, improving the chances of successful conception and pregnancy.